Vaccination continues to be one of the most powerful and evidence-based tools in modern medicine. As scientific understanding evolves, so does the UK’s national schedule. From January 2026, several important updates will come into effect, reshaping how and when both children and adults are protected.
At The Sloane Street Surgery, we have long taken a proactive, personalised, evidence-led approach to vaccination, rather than sticking rigidly to the UK vaccination schedule, often introducing vaccines well before they entered the NHS schedule. Many of our patients have had some of their vaccines abroad and spend their time between different countries, making an individualised approach all the more important.
Below we answer some common questions about what’s changing, why it matters, and how we can help ensure your family’s vaccination record is complete.
What’s changing in the UK childhood vaccination schedule in 2026?
From January 2026, the UK’s childhood vaccination programme will include:
- A new 18-month appointment
• A fourth dose of the 6-in-1 vaccine (protecting against diphtheria, tetanus, pertussis, polio, Hib, and hepatitis B)
• The second MMR dose, moved earlier from 3 years 4 months
• The introduction of the combined MMRV vaccine – providing protection against measles, mumps, rubella, and now chickenpox, which becomes routine for the first time in the UK - Earlier protection against Meningitis B
The second MenB dose is moved from 16 weeks to 12 weeks, after evidence showed most infant cases now occur before four months of age. - Discontinuation of the Hib/MenC vaccine (Menitorix®)
This is because the manufacturer has ceased production and there is no licenced alternative. Instead, protection is achieved as follows:- MenC protection is maintained through the teenage MenACWY booster, which provides strong herd immunity.
- Hib protection is reinforced through the additional 6-in-1 booster at 18 months.
Why has the childhood schedule been redesigned?
The Joint Committee on Vaccination and Immunisation (JCVI) reviewed national disease data and found several opportunities to improve protection and simplify delivery:
- Meningococcal B disease now occurs earlier in infancy, hence the shift of the second dose to 12 weeks.
- Immunity to measles, mumps and rubella is strengthened by giving the second dose earlier.
- Hib immunity wanes in toddlers, so an 18-month booster maintains long-term protection.
- The inclusion of chickenpox (MMRV) brings the UK in line with countries such as the US, Canada and Australia, where varicella vaccination has reduced hospitalisations and complications.
- The new 18-month visit provides a structured opportunity to catch up on missed doses, improving overall vaccine uptake.
How does the UK schedule compare with other countries?
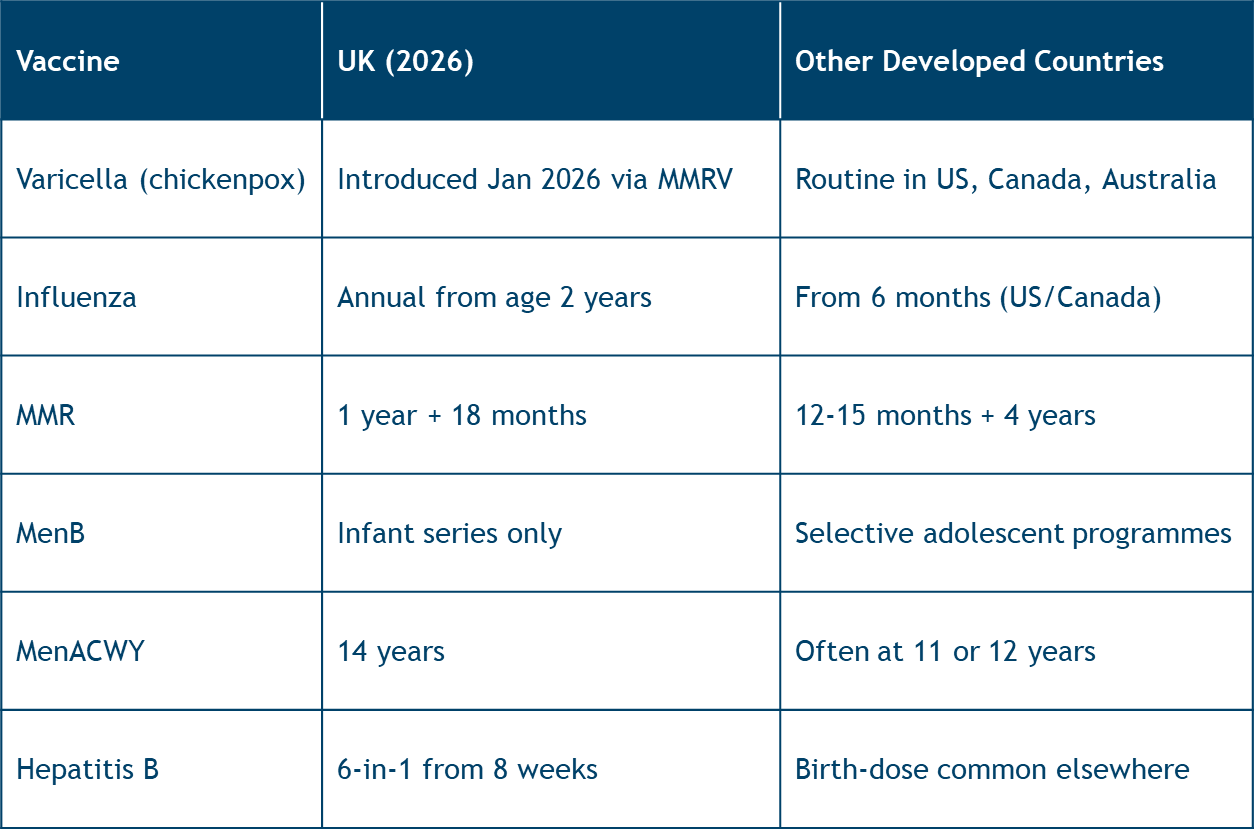
The UK remains at the forefront of evidence-driven immunisation, with timing optimised for local epidemiology and programme effectiveness.
Should the MenACWY vaccine be given earlier?
In some countries, MenACWY is given at 11–12 years, offering earlier adolescent protection before increased social contact.
In the UK, it is currently given at 14 years (usually alongside the teenage tetanus/diphtheria/polio booster).
However, for pupils entering boarding school or students preparing for university or overseas study, an earlier MenACWY dose should be considered. We are happy to advise on this individually.
What about the teenage DTP booster?
All teenagers should receive a tetanus, diphtheria and polio (Td/IPV) booster at around 14 years.
This maintains long-term protection into adulthood. Those who miss it at school can receive it at the surgery at any time later.
Should teenagers have a MenB booster?
Invasive meningitis B is a devastating infection that kills around 10% of sufferers. 25 % of those who survive have life altering complications such as loss of limbs or neurological damage.
MenB antibodies from infancy wane over time. A booster in adolescence produces a strong response and could protect against the smaller second peak in meningococcal disease seen in older teenagers.
While not yet routine, the JCVI is reviewing this evidence.
We already offer MenB boosters for those at higher risk — such as students entering halls, travellers to endemic regions, or individuals wishing for the highest level of protection.
Why is HPV now 1 dose for most teenagers?
HPV vaccination protects against the viruses that cause cervical cancer and genital warts. Boys and girls both receive this aged 12/13. This used to be a 2 or 3 dose schedule but major public health authorities in the UK and globally now endorse the one dose schedule. Although a 2 dose schedule produces higher antibody levels, the benefit of this is unclear because one dose antibody levels remain protective. We are happy to administer a one or two dose schedule at the surgery.
Flu vaccination for children: who needs what and when?
The nasal flu vaccine or flu injection is routinely offered to children from age 2 years (the nasal flu vaccines is currently only available in the NHS and we can only give the injection in the surgery.)
However, infants aged 6 months–2 years can receive the injected inactivated flu vaccine privately.
Importantly, babies under 2 receiving flu vaccine for the first time need two doses, given four weeks apart, during their first flu season to achieve adequate protection.
What are the main vaccines recommended for adults?
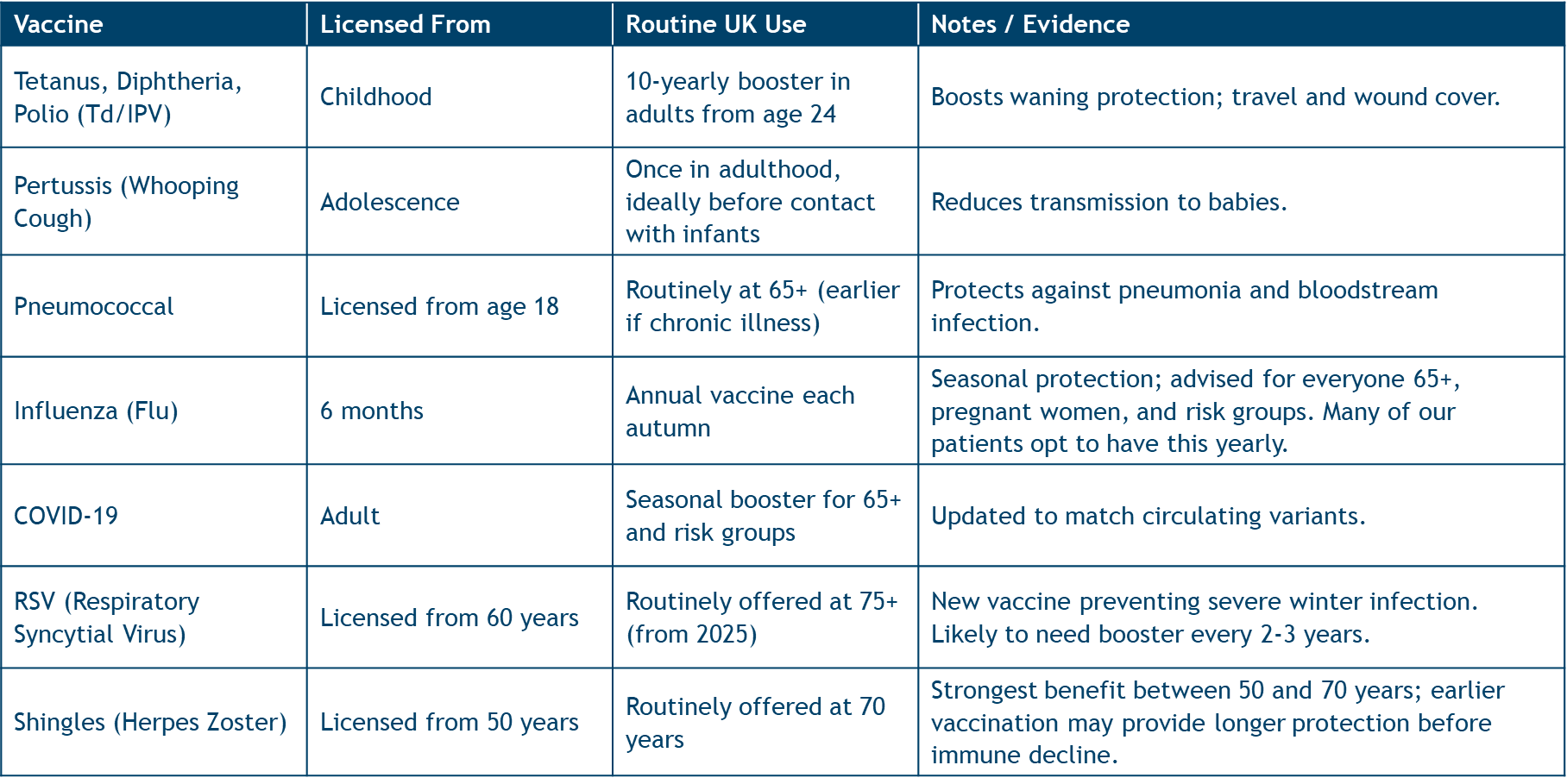
What do we know about the new RSV vaccine and boosters?
RSV (Respiratory Syncytial Virus) is a common winter infection that can cause severe illness in older adults and babies.
The first RSV vaccines for adults were approved in the UK in 2024, licensed from age 60 and now offered routinely from age 75.
Current studies show protection lasting at least two years, though antibody levels wane over time. It is likely that booster doses every 2–3 years will eventually be recommended, particularly for those over 75 or with chronic lung or heart disease. We will update our patients as guidance evolves.
How can I check my or my child’s vaccination record?
Many of our patients have international or incomplete vaccination histories. At The Sloane Street Surgery, we offer:
- A comprehensive vaccine review service combining NHS and overseas records (please provide us with all records you possess.)
- A tailored catch-up plan to ensure full protection
- Antibody testing when documentation is unclear — for example, to confirm immunity to measles, mumps, rubella, varicella or hepatitis B
This service helps ensure that you and your family are protected to the highest standard, wherever your previous vaccines were given.
Summary: UK Routine Schedule from January 2026
Infant & Early Childhood

Adult
- Tetanus/diphtheria/polio: Every 10 years
- Pneumococcal: From 65+ (or earlier if indicated)
- Influenza: Annually each autumn
- COVID-19: Seasonal booster for 65+ and risk groups
- RSV: From 75+ (licenced from aged 60)
- Shingles: From 70 (routinely), licensed from 50
Final Thoughts
These updates reflect the UK’s ongoing commitment to evidence-based prevention – providing earlier and broader protection in infancy and more comprehensive coverage across adulthood.
At The Sloane Street Surgery, we remain ahead of the curve in adopting safe, effective vaccination strategies. If you’d like us to review your vaccine history, arrange antibody testing, or discuss additional vaccines such as an early MenACWY or MenB booster, please contact us to book a consultation.
About the author

MBBS BSc MRCGP DFSRH
“We have the luxury of time, both to spend with our patients in consultation and afterwards, to ensure their medical needs are met quickly and efficiently and by the right person”.
Having worked in multiple specialities across London hospitals, my particular interests now lie in paediatric and teenage care, women’s health, acute medicine, disease prevention and psychiatry.
I enjoy all aspects of General Practice but particularly looking after whole families: from newborns to grandparents, helping people when they need it most, quickly, efficiently, and kindly.